Author: Gina Rogers,
Published On: January 21, 2019
This article originally appeared on American Nurse Today
This study investigated the use of aromatherapy in the workplace to reduce nurse stress.
Takeaways:
- Essential oil (aromatherapy) uses “naturally extracted aromatic essences from plants to balance, harmonize, and promote the health of body and mind.”
- Aromatherapyhas gained popularity as a safe and cost-effective complementary therapy to alter mood and physical symptoms.
- Two nurse-driven aromatherapy studies indicated decreased staff perception of stress and increased mood. Patients experienced decreased agitation.
By Juli Reynolds, BSN, RN; Betsy Parker, RN; Nancy Wells, DNSc, RN, FAAN; Elizabeth Card, MSN, APRN, FNP-BC, CPAN, CCRP
Aromatherapy is an age-old therapy designed to alter mood and physical symptoms. It has gained popularity as a safe and cost-effective complementary and alternative therapy. As the evidence of aromatherapy’s effectiveness has grown, nurses have increased the use of essential oils to manage their own stress as well as their patients’ stress and anxiety.
This article describes the basics of aromatherapy and two institutional review board–approved studies to build on the evidence of the positive benefits of essential oils for both nurses who work in clinical settings and their patients.
Essential oils primer
According to the National Association for Holistic Aromatherapy, essential oil therapy (aromatherapy) is “the art and science of utilizing naturally extracted aromatic essences from plants to balance, harmonize, and promote the health of body and mind.” Essential oils are volatile, aromatic compounds found in various parts of plants, including stems, leaves, roots, and seeds. Thousands of essential oils have been identified; each is unique and contains hundreds of chemical components. Selecting the appropriate oil depends on the desired therapeutic effect; their versatility allows for options based on preference and application. All therapeutic-grade oils meet criteria that include indigenous sourcing for potency and stringent purity testing.
Essential oils can be used internally, topically, or aromatically. For the purpose of our studies, we chose an aromatic model—scent dispersed into the air via a diffuser. Through our sense of smell, essential oils affect our physiology, emotions, and behavior by stimulating hormones and neurotransmitters. Aromatic use is highly effective and can be applied to any of the essential oils in moderation. Previously, scientists had underestimated the influence aroma can have on health. Recent research supports the beneficial effect essential oils have on physical symptoms as well as emotional states. (See Recent research.)
Recent researchHere’s a sampling of essential oils and their effects on common symptoms. Respondents rated the essential oil on a 0-to-10 scale.
Source: Johnson et al. 2016 |
Because essential oils are produced from plants, they’re grouped into classes based on plant type. Plants from the same class produce similar responses. (See Classifying essential oils.)At the root of these similarities is the chemistry of the essential oils, which can be used to determine what oils to use for a specific effect.
Classifying essential oilsEssential oils are grouped into classes based on plant type. Oils within each class have similar effects.
|
Study rationale
The evidence suggests that people can use scents that consistently produce specific responses to improve emotional and/or physical well-being. Our research question was: Does diffusing essential oils that promote relaxation and balance affect the nursing staff’s stress level? Limited evidence exists on the influence of nurse stress on patient stress, so we took the opportunity to explore the possible impact of nurse stress on patient stress as indicated by changes in blood pressure and use of sedatives to reduce anxiety and agitation.
Perioperative project
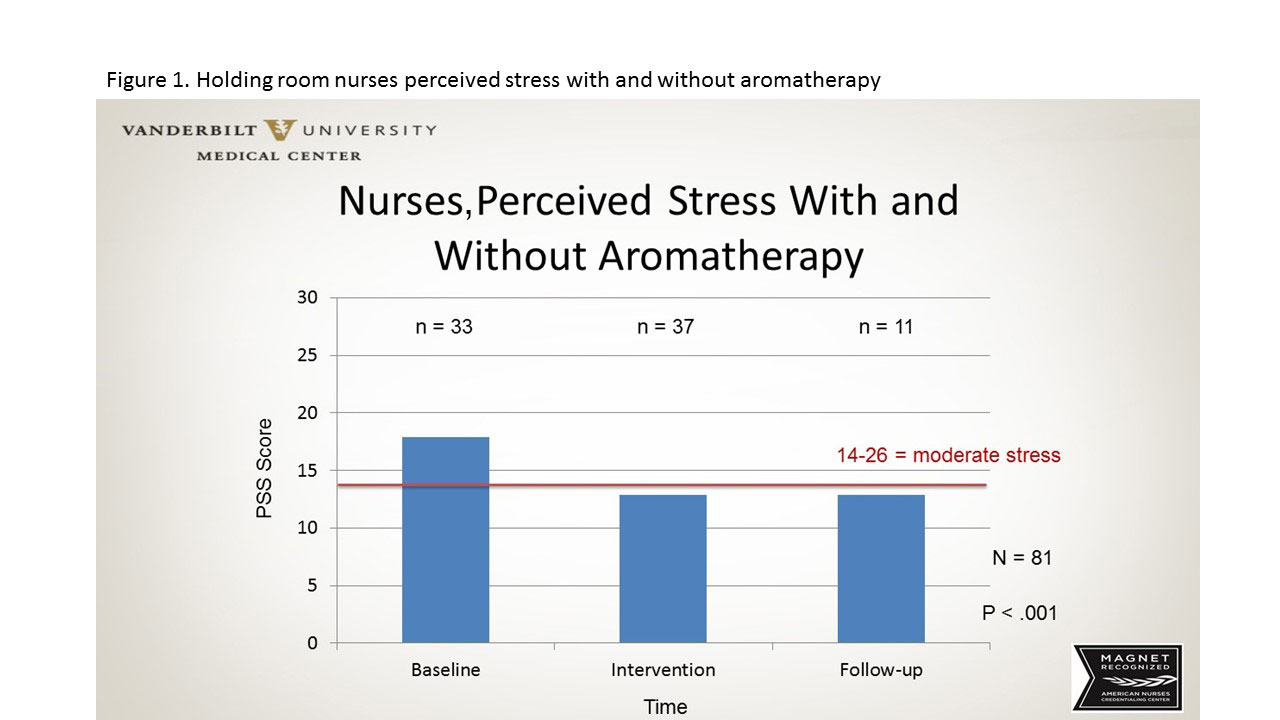
Using an electronic survey, we obtained participating nurses’ stress levels before, during, and after diffusing essential oils in the main preoperative holding room at an urban level-one academic medical center. Stress was measured with the Perceived Stress Scale (PSS), a 10-item scale with a 5-point Likert response format. The PSS is a valid and reliable measurement tool. Thirty-three nurses completed the presurvey in the 2 weeks before the intervention was started. Nebulizing diffusers were then placed at the nurses’ station for aromatherapy over the next 4 weeks. All essential oils used were citrus based and single oil (no blends). Scents included lime, wild orange, grapefruit, tangerine, and lemon. The purity and quality of the oils was determined using gas chromatography and mass spectrometry. All oils were indigenously sourced from a single harvest.During the 4 weeks, 37 nurses completed the PSS.
The diffusers were then removed, and over the next 4 weeks, 11 participants completed the PSS. Analysis revealed a statistically significant reduction in perceived stress levels from baseline to during and after aromatherapy (P< .001) in the holding room staff. (See Perioperative project: Nurse-perceived stress.) Of equal importance, no adverse events were reported by staff, patients, or families when the diffusers were placed in a common area of the perioperative holding room.
Perioperative project: Nurse-perceived stress
This figure illustrates nurses’ perceived stress before and after aromatherapy intervention.
Palliative care project
In our second study, we examined the impact of aromatherapy on staff stress and anxiety in a palliative care environment, where nurses care for patients with serious life-threatening diseases and difficult-to-manage symptoms. In addition, we explored the impact that staff stress might have on patient stress.
Four weeks before essential oil diffusion, 28 nurses completed an anonymous, electronic stress and mood questionnaire. We selected a blend of wood, frankincense, blue tansy, blue chamomile, and spruce, all of which are known for their grounding and balancing qualities. Oil purity and quality were determined using gas chromatography and mass spectrometry. All oils were indigenously sourced from a single harvest.
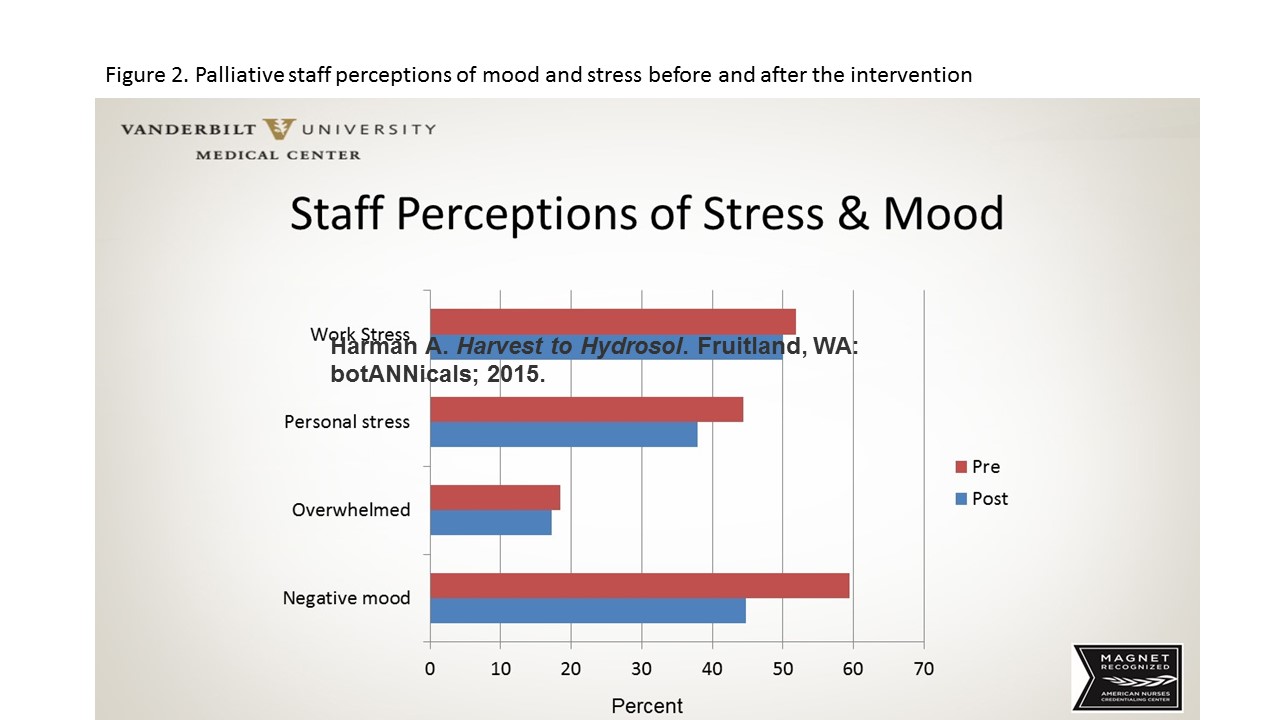
The essential oil was continuously diffused for 4 weeks in nursing stations located in the unit hallway. At the end of the 4 weeks, we sent an electronic postintervention questionnaire. The staff reported an increase in positive mood, a decrease in stress, and an improvement in feeling “more grounded.” (See Palliative project: Nurse-perceived stress.)
Palliative project: Nurse-perceived stress
This figure illustrates nurses’ perceptions of mood and stress before and after aromatherapy intervention.
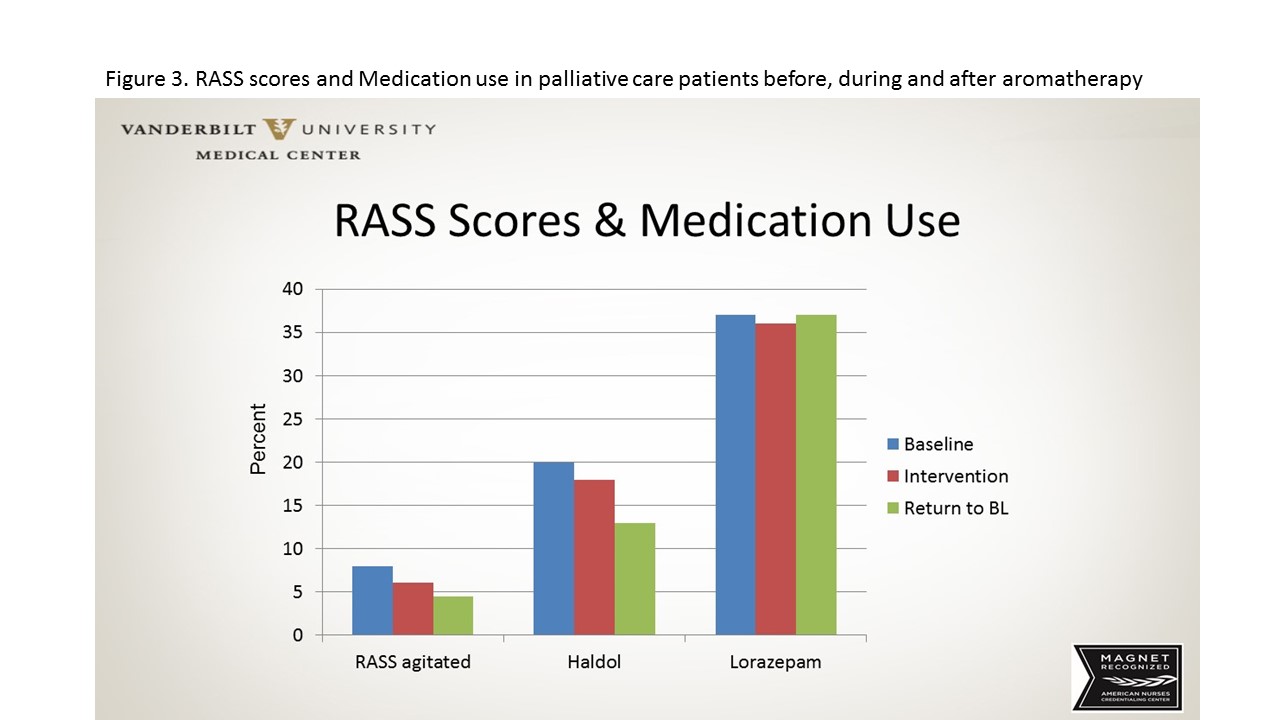
This information led us to ask whether the nurses’ reduced stress would impact the patients in their care. We selected several patient outcomes that would reflect patient stress and anxiety, including blood pressure variability, Richmond Agitation–Sedation Scale (RASS) scores, haloperidol administration for agitation, and lorazepam administration for anxiety. Patient data from electronic health records (EHR) were evaluated for 3 months—before, during, and after the intervention. We found significantly less blood pressure variability during and after the intervention. We interpret this as an overall lower stress level in the patients admitted to palliative care during and after aromatherapy diffusion in the nurses’ work areas. We also saw a decrease in RASS scores and haloperidol administration, suggesting a positive effect of decreased patient stress. Little change in lorazepam administration occurred during the study. (See Patient stress and anxiety.)
Patient stress and anxiety
Richmond Agitation–Sedation Scale (RASS) scores and medication administration were used to measure palliative care patient stress before, during, and after aromatherapy intervention.
Positive impact
Based on our review of the literature and experience with these projects, we found that essential oils have a positive impact on staff perceptions of stress in a busy workplace. In addition, we found no reports of adverse events during the essential oil diffusion in either of the clinical areas we studied. Findings from the EHR should be viewed with caution. Although positive effects were seen on certain patient outcomes—such as blood pressure variability—the study wasn’t designed to examine cause and effect. It does, however, raise questions about the interplay between nurses’ emotional state and patient response.
These studies demonstrate the beneficial effect aromatherapy can have on nurses in the workplace. Many essential oils are inexpensive (although costs vary and some may cost over $100 per ounce), making them a cost-effective, safe, natural, and pleasant intervention for nurses and other healthcare staff.
The staff members who designed the intervention experienced a sense of empowerment associated with taking a nontraditional idea, developing it into a plan of action, and implementing a successful program. These results have led to excitement about the power and potential of essential oils in patient care settings.
Both studies have provided evidence about the impact of aromatherapy on staff stress and some indication that a more relaxed staff nurse might transmit that calm balance when providing patient care. These findings also highlight the need for aromatherapy research and education. We’re currently working on an education initiative and a follow-up research project involving patient care.
Juli Reynolds is an RN 4 in perioperative services at Vanderbilt University Medical Center in Nashville, Tennessee. Betsy Parker is an RN 2 in clinical research at Vanderbilt University Medical Center. Nancy Wells is a research professor at Vanderbilt University school of nursing. Elizabeth Card is a nursing research consultant and nurse practitioner at Vanderbilt University Medical Center.
Selected references
Berger L, Tavares M, Berger B. A Canadian experience of integrating complementary therapy in a hospital palliative care unit. J Palliat Med. 2013;16(10):1294-8.
Buckle J. Clinical Aromatherapy: Essential Oils in Healthcare. 3rded. London, England: Churchill Livingstone; 2015.
Harman A. Harvest to Hydrosol: Distill Your Own Exquisite Hydrosols at Home. Fruitland, WA: Botannicals; 2015.
JohnsonJR,RivardRL,GriffinKH, et al.The effectiveness of nurse-delivered aromatherapy in an acute care setting. Complement Ther Med. 2016;25:164-9.
Joswiak D, Kinney ME, Johnson JR, et al. Development of a health system-based nurse-delivered aromatherapy program. J Nurs Adm. 2016;46(4):221-5.
Lee EH. Review of the psychometric evidence of the perceived stress scale. Asian Nurs Res. 2012;6(4):121-7.
Valnet J, Tisserand RB. The Practice of Aromatherapy: A Classic Compendium of Plant Medicines and Their Healing Properties. Rochester, VT: Healing Arts Press; 1990.
Varney E, Buckle J. Effect of inhaled essential oils on mental exhaustion and moderate burnout: A small pilot study. J Altern Complement Med. 2013;19(1):69-71.